I am not a medical doctor. I know a few, and they are all awesome! But I am not one. Nor am I a healthcare professional of any kind.
These updates are my way of helping everyone sift through the riff-raff. There is a lot of misinformation floating around. My goal with these posts is to pass along relevant information from the medical community – direct from the source – with some translation into regular English.
I want to keep you informed as best as I can.
Latest Numbers
Total United States cases: 7.038
— Travel-related: 269
— Close contact: 276
— Under investigation: 6,493
Total deaths: 97
States reporting cases: 50 states, District of Columbia, Puerto Rico, Guam, and US Virgin Islands
(Numbers pulled from other reliable resources) Total United States cases reported by other medical sites:
Johns Hopkins:
Total cases: 9,415
Total deaths: 150
Total recovered: 106
Higher totals may be reported by other news agencies. This information is pulled straight from official government / medical university websites only. The numbers may conflict. If I understand things correctly, the CDC site is pulled from reports they receive by noon while Johns Hopkins pulls in data continuously.
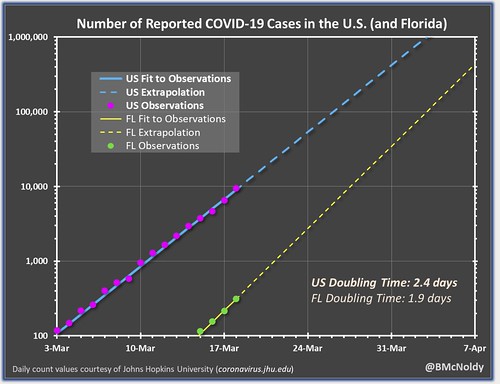
Brian McNoldy, Senior Research Associate at Univ. of Miami’s Rosenstiel School, put that chart together. As it notes, it is pulling numbers from the Johns Hopkins totals. It shows teh double-time of cases as about two-and-a-half days.
New Research
Coronavirus lingers on surfaces
The National Institute of Health reported that a new paper published in the New England Journal of Medicine shows the Coronavirus can survive on surfaces for longer than originally anticipated.
The virus that causes coronavirus disease 2019 (COVID-19) is stable for several hours to days in aerosols and on surfaces, according to a new study from National Institutes of Health, CDC, UCLA and Princeton University scientists in The New England Journal of Medicine. The scientists found that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was detectable in aerosols for up to three hours, up to four hours on copper, up to 24 hours on cardboard and up to two to three days on plastic and stainless steel.
The results provide key information about the stability of SARS-CoV-2, which causes COVID-19 disease, and suggests that people may acquire the virus through the air and after touching contaminated objects. The study information was widely shared during the past two weeks after the researchers placed the contents on a preprint server to quickly share their data with colleagues.
Since other studies have found that the Coronavirus is spreading between people who are pre-symptomatic, this may help researchers understand the speed of the spread. And since researchers at Johns Hopkins found that the incubation period is between five and 14 days, this means those infected can be leaving the virus on surfaces for up to 14 days before said person even knows they are sick.
Certain blood types may – may! – be at risk
I’ve had a few questions from folks recently about certain blood types being at a higher risk for COVID-19. A new research paper that is in pre-print and is not yet peer-reviewed is getting a lot of traction on the web. The paper titled, “Relationship between the ABO Blood Group and the COVID-19 Susceptibility” tries to make a connection between blood type and COVID-19 infections.
In the paper, the authors note:
The ABO group in 3694 normal people in Wuhan showed a distribution of 32.16%, 24.90%, 9.10% and 33.84% for A, B, AB and O, respectively, versus the distribution of 37.75%, 26.42%, 10.03% and 25.80% for A, B, AB and O, respectively, in 1775 COVID-19 patients from Wuhan Jinyintan Hospital. The proportion of blood group A and O in COVID-19 patients were significantly higher and lower, respectively, than that in normal people (both P < 0.001). Similar ABO distribution pattern was observed in 398 patients from another two hospitals in Wuhan and Shenzhen. Meta-analyses on the pooled data showed that blood group A had a significantly higher risk for COVID-19 (odds ratio-OR, 1.20; 95% confidence interval-CI 1.02~1.43, P = 0.02) compared with non-A blood groups, whereas blood group O had a significantly lower risk for the infectious disease (OR, 0.67; 95% CI 0.60~0.75, P < 0.001) compared with non-O blood groups.
This new research cites older research as a starting point. The older paper paper, titled, “Blood Groups in Infection and Host Susceptibility” discusses the SARS outbreak and how a certain group of people – in a small sample – were infected.
Like other human coronaviruses, SARS-CoV infects the mucosal epithelium, causing an acute respiratory illness often accompanied by gastroenteritis. In a Hong Kong outbreak, there was an apparent association between disease transmission and ABO type. An epidemiology study of 34/45 hospital workers who contracted SARS after exposure to a single index patient showed that most of the infected individuals (23/34) were non-group O individuals (groups A, B, and AB). Group O individuals were relatively resistant to infection, with an OR of 0.18 (95% CI, 0.04 to 0.81; P = 0.03).
In short, both the new research and the older research suggest Blood Type A, B and AB had a higher rate of infection than those with Type O.
Before you get too concerned, or breathe a sigh of relief… The new research is not yet peer-reviewed and the old research was one, single and very small, study. On a similar, but not the same, virus.
Might be tough to tell if your child is infected
In a new study from a children’s hospital in China, only 40-percent of kids who had COVID-19 registered a fever. Nearly 60-percent had a fever less than 100-degrees. And said fever only lasted three days.
Other symptoms were cough (only about 50-percent had one), throat inflammation (only about 45-percent had this), and an increased heart rate (about 40 percent had this).
About 15-percent of kids showed zero symptoms. That means some children can have it, pass it along, and get better, without even knowing they are/were ever sick.
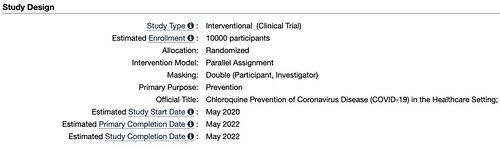
New clinical trial begins on treatment
The study, titled, “Chloroquine Prevention of Coronavirus Disease (COVID-19) in the Healthcare Setting” is set to begin in May. Because trials are just starting, I couldn’t find data on any treatments that have already used this drug. The researchers behind the study note:
The study is a double-blind, randomised, placebo-controlled trial that will be conducted in health care settings. After obtaining fully informed consent, the investigator will recruit healthcare workers, or other individuals at significant risk who can be followed reliably for 5 months. 10,000 participants will be recruited and the investigator predict an average of 200 participants per site in 50 sites.
The participant will be randomised to receive either chloroquine or placebo (1:1 randomisation). A loading dose of 10mg base/kg, followed by 150 mg daily (250mg chloroquine phosphate salt) which will be taken for 3 months or until they are diagnosed with COVID-19. Subsequent episodes of symptomatic respiratory illness, including symptomatic COVID-19, clinical outcomes, and asymptomatic infection with the virus causing COVID-19 will be recorded during the follow-up period.
But, don’t look for Chloroquine to be widely administered to patients any time soon.
The clinical trial ends in May. Of 2022.
How fast does it spread?
That means there may not be a treatment for awhile and we need to rely on our actions to help prevent the spread.
COVID19 has an R0 value of between 2 and 3. That means for every one person that has it, that person can spread it to someone else. For reference, the regular flu R0 value is a 1.3, meaning you pass the flu on to one other person.
The higher R0 value creates the possibility for exponential growth. But, only under the right conditions as highlighted by a published paper titled, “Early dynamics of transmission and control of COVID-19: a mathematical modelling study.”
Even if the reproduction number is as high as in Wuhan in early January, it could take several introductions for an outbreak to establish, because high individual-level variation in transmission makes new chains of transmission more fragile, and hence it becomes less likely that a single infection will generate an outbreak. This factor highlights the importance of rapid case identification and subsequent isolation and other control measures to reduce the chance of onward chains of transmission.
We estimated that the median daily reproduction number (Rt) in Wuhan declined from 2·35 (95% CI 1·15-4·77) 1 week before travel restrictions were introduced on Jan 23, 2020, to 1·05 (0·41-2·39) 1 week after. Based on our estimates of Rt, assuming SARS-like variation, we calculated that in locations with similar transmission potential to Wuhan in early January, once there are at least four independently introduced cases, there is a more than 50% chance the infection will establish within that population.
The take-away from that is that four independentncases in a population show a 50-50 chance it will become established. That may feel scary. However, the researchers also found that once restrictions were in place – and followed – it trimmed the transmission rate down to below the regular flu.
But the restrictions – self isolation, social distancing, etc – are pretty strict. And it remains to be seen if the United STates will implement such restrictions.
What should I do, right now?
I know. It can seem overwhelming with the amount of information and updates flying around. But I think it is best to follow the CDC’s guidance at this point.
— Know where to get your local / state-level information
For Mississippi: https://msdh.ms.gov/msdhsite/_static/14,0,420.html
For Louisiana: http://ldh.la.gov/Coronavirus/
For Alabama: http://www.alabamapublichealth.gov/infectiousdiseases/2019-coronavirus.html
If you live in a state outside of the region, head to google and type in, “dept of health” followed by whatever state you live. Google should take you to that state’s department of health and on the main page, most states have a link to an update on the Coronavirus.
— Know the Symptoms
Look for things like a fever, dry cough, and shortness of breath. But also know when it may become an emergency. It becomes an emergency when you have difficulty breathing, a persistent pain or pressure in the chest, you develop general confusion, and if you develop bluish lips or face.
Also recognize that body aches, weak stomach, nasal congestion, a sore throat, and other symptoms of the regular flu are not the same as the symptoms with Coronavirus.
— Stay home when you are sick
Any kind of sick. If you feel like you may have Coronavirus, call your health care provider’s office in advance of a visit. If you have any sickness, the CDC recommends to limit movement in the community, limit visitors, and practice good social distancing.
— Know if you are at a higher risk
Know what additional measures those at higher risk and who are vulnerable should take. Those at higher risk include older adults (over 60), people who have serious chronic medical conditions (like heart disease, diabetes, lung disease). Some research has indicated that people with asthma may also be included in the higher risk category.
— Take steps to mitigate your infection
The CDC recommends to “Implement steps to prevent illness” by washing high-traffic areas more often, washing hands with soap and water and if someone is sick, to isolate the sick person into a low-traffic area of the home.
— Create a Household Plan
Create a household plan of action in case of illness in the household or disruption of daily activities due to COVID-19 in the community.
A note for those fighting cancer during this pandemic
The Mayo clinic has been doing an excellent job at keeping new info posted on their website for folks curious about this virus. They had a few quotes from Dr. Rafael Fonseca, a hematologist and interim executive director of the Mayo Clinic Cancer Center, for those fighting cancer.
“Cancer is a very broad word and could encompass a relatively minor cancer with perhaps no implications or no difference from someone who is otherwise healthy with regards to COVID-19 to a more extreme situation where a patient with cancer might be facing a situation of a more advanced disease or a treatment that might be more immunosuppressive, that is, that would bring the immune system down more than average and then, particularly in those groups of patients, we might think of a different way to approach their care.”
“Furthermore, some treatments may affect different how a person may be able to fight off an infection or not,” says Dr. Fonseca. “Some of the treatments that bring down a certain type of white cells create what we call myelosuppression, that is, the neutrophils are down. That is usually thought of to be more important for bacterial infections. Some other cancer treatments may affect more the way our immune system responds, and there’s a number of cells there like the lymphocytes. So maybe that’s more important for viruses. But this is all speculative because we really don’t have information at this point.”
It is important, according to the May Clinic, to keep in contact with your oncologist about the best steps for your specific cancer and your specific treatment plan.
In general, the Mayo Clinic says to consider these tips to reduce the potential for infection:
– Avoid contact with people who are sick.
– Practice social distancing.
– Wash your hands often with soap and water, or use an alcohol-based hand sanitizer.
– Avoid touching your eyes, nose and mouth if your hands aren’t clean.
– Determine who can care for you if you become ill.
– Also, consider these recommendations for supplies:
-Contact your health care provider to ask about obtaining extra necessary medications in case you need to stay home for a prolonged period of time.
– If you cannot get extra medications, consider using mail-order for medications.
– Be sure you have over-the-counter medicines and medical supplies, such as tissues, to treat fever and other symptoms. Most people will be able to recover from
– Have enough household items and groceries on hand so that you will be prepared to stay at home for a period of time.
Here is a quick podcast from the NEJM. It is an interview with Dr. Eric Rubin and Dr. Lindsey Baden on new research on possible treatments for Covid-19. I’ll be honest, it is a bit heavy on medical verbiage and I had to stop it and rewind it a few times when listening. But it is worth the time. Especially if you are at home, practicing social distancing.
The doctors talk about a lot of good information, but at one point, they bring up a very good point. Baden says, “… The ability to determine, systematically, if a new therapy works, was very difficult given the conditions the providers are in…” and I think that is an important thing to remember right now.
It is very hard to test new drugs and new treatments because of the situation people are in when they enter the hospital and the numbers of people who are being treated, and the treatments those people need. Unlike a “simple” clinical trial test, where you get volunteers and the timetable isn’t as dire, in the middle of a pandemic that is not the case. And it can be difficult for CVOID-19 research to get done.