Quick reminder: I’m not a doctor. For specific questions about your specific health, always consult your doctor, not the internet. Not some guy you know. Not a facebook post. Your doctor. The person who specializes in knowing about how the human body works.
And even though I am not a doctor, these posts are an attempt to be a conduit for new information to keep you updated on the latest numbers, research and information directly from the CDC, WHO, and the medical community.
Latest Numbers
WHO Numbers
Total Worldwide Cases: 1,133,758
Total Worldwide Deaths: 62,784
CDC Numbers
Total United States cases: 204,826
— Travel-related: 1,388
— Close contact: 4,325
— Under investigation: 233,566
Total deaths: 7,616
States reporting cases: 50 states, District of Columbia, Puerto Rico, Guam, the Northern Mariana Islands, and the U.S. Virgin Islands
COVID-19 cases reported by other medical sites:
Johns Hopkins
Total Worldwide Cases: 1,273,794
Total Worldwide Deaths: 69,419
Total Worldwide Recovered: 260,193
Total US cases: 337,072
Total US deaths: 9,633
Total US recovered: 17,448
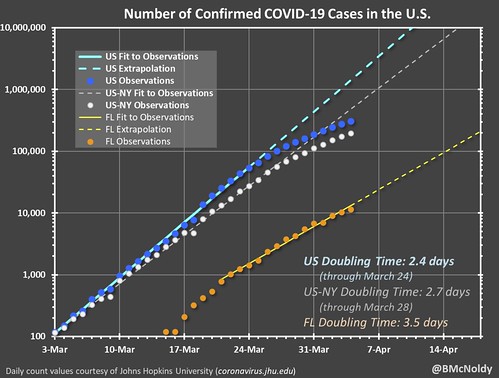
Brian McNoldy, Senior Research Associate at Univ. of Miami’s Rosenstiel School, put a chart together of the growth. As it notes, it is pulling numbers from the Johns Hopkins totals.
Regional Numbers
| Cases | Tested | Deaths | %-positive | Mortality Rate | |
| MS | 1638 | N/A | 43 | N/A | 2.63% |
| LA | 13010 | 55957 | 477 | 23.25% | 3.67% |
| AL | 1841 | 13108 | 45 | 14.04% | 2.44% |
| TN | 3633 | 45300 | 44 | 8.02% | 1.21% |
| AR | 853 | 11780 | 16 | 7.24% | 1.88% |
| Total | 20975 | 126145 | 625 | 16.63% | 2.98% |
A few states in the region do release the number of hospitalized people due to COVID-19. Those numbers are as follows:
Mississippi: 312
Louisiana: 1,803 (561 on ventilators)
Alabama: 231
Tennessee: 328
Arkansas: Not given
Making Estimates from past research
I talked about research from the Cruise Ships that may be relevant to estimating the number of cases without testing everyone (since that isn’t a feasible option). Plus, this type of estimate would make a good “first guess” at the number of asymptomatic people (the people who don’t feel sick, but are still infected), too.
This type of estimating isn’t perfect. In fact, it is far from it. And it is just an estimate. But based on the past research, it is at least a start.
| Estimated Symptomatic | Estimated Asymptomatic | Estimated total | |
| MS | 2498 | 548 | 3047 |
| LA | 19843 | 4356 | 24199 |
| AL | 2808 | 616 | 3424 |
| TN | 5541 | 1216 | 6757 |
| AR | 1301 | 286 | 1587 |
| Total | 31991 | 7022 | 39014 |
New research
A tiger has Coronavirus
There are reports out from the National Geographic that a tiger at the Bronx Zoo has been infected with Coronavirus. This possibility was postulated by researchers more than a month ago. A recent paper, that is still
You may remember reading – back on February 29th – on this blog:
The original study suggested that animal-to-animal transmission was possible but animal-to-human and vice-versa was unlikely with the mentioned aniumals.
It would seem, if this news is true, that isn’t the case anymore.
Some patients re-testing positive after given “clean bill of health”
In a paper out of China titled, “SARS-CoV-2 turned positive in a discharged patient with COVID-19 arouses concern regarding the present standard for discharge” researchers at University of Chinese Academy of Sciences report an asymptomatic discharged patient who recovered from COVID-19 was re-tested as positive for SARS-CoV-2, which “arouses concern regarding the present discharge standard” of COVID-19.
I’m still trying to wrap my head around this one, but it seems like in certain scenarios (but not all, by any means) there are people who have no fever, reduced symptoms, clear chest x-rays, and are “negative” on a swab for more than 48 hours… who then at a later point test positive again.
The researchers suggest that “nucleic acid detection has a certain possibilities of false negative, which would mainly depend on the following situations: (1) the source of samples collected; (2) the method of samples collected; (3) antiviral drugs or hormone taken; (4) the sensitivity of nucleic acid test kit.”
It seems that false-negative tests with COVID-19 are more prevalent than false-positive tests.
Old drug, new tricks
A paper in the Journal of Antiviral Research that is in pre-release shows that an old drug used to fight off parasites may be useful against COVID-19. The paper, titled, “The FDA-approved Drug Ivermectin inhibits the replication of SARS-CoV-2 in vitro” highlights that Petri dish research shows that this drug is reasonably effective at halting a new infection within 48 hours.
From the paper:
To test the antiviral activity of ivermectin towards SARS-CoV-2, we infected Vero/hSLAM cells with SARS-CoV-2 isolate Australia/VIC01/2020 at an MOI of 0.1 for 2 h, followed by the addition of 5 μM ivermectin. Supernatant and cell pellets were harvested at days 0-3 and analysed by RT-PCR for the replication of SARS-CoV-2 RNA (Fig. 1A/B). At 24 h, there was a 93% reduction in viral RNA present in the supernatant (indicative of released virions) of samples treated with ivermectin compared to the vehicle DMSO.
Similarly a 99.8% reduction in cell-associated viral RNA (indicative of unreleased and unpackaged virions) was observed with ivermectin treatment. By 48h this effect increased to an ∼5000-fold reduction of viral RNA in ivermectin-treated compared to control samples, indicating that ivermectin treatment resulted in the effective loss of essentially all viral material by 48 h.
While this may seem very promising, this paper still has to go through more scientific peer review. And until then, the findings should treated as such – non-peer-reviewed.
Four-drug attack
In the same Journal, a paper titled, “Remdesivir, lopinavir, emetine, and homoharringtonine inhibit SARS-CoV-2 replication in vitro” was published on April 3rd. It gets pretty ‘medical-y’ at times. But the researchers found that Remdesivir inhibits SARS-CoV-2 replication in Vero-E6 cells, Lopinavir but not ritonavir inhibits SARS-CoV-2 replication with EC50, and Homoharringtonine and emetine inhibits SARS-CoV-2 replication with EC50. Combination of remdesivir and emetine showed synergistic effect in vitro.
They also offered a quick synopsis, saying:
We confirm the antiviral activity of four compounds that have been reported to inhibit other coronavirus or SARS-CoV-2 replication in vitro. Our results suggest that combinational therapy may help to reduce the effective concentration against SARS-CoV-2 under the maximal therapeutic plasma concentration. There is an urgent research need to identify optimal dose combination of effective compounds against the SARS-CoV-2 virus for better clinical benefit.
Pregnancy and COVID-19
A pre-print of a paper titled, “COVID-19 in pregnancy: early lessons” from the American Journal of Obstetrics & Gynecology highlights a, perhaps, unanticipated problem. Researchers at Columbia University in New York City followed the cases of seven women with COVID-19 that recently gave birth and the effects and after-effects of their illness with respect to their pregnancy.
This limited initial US experience suggests a need for immediate changes in obstetric clinical practice. Two of seven (28.6%) confirmed COVID-19-positive patients in this early series were asymptomatic upon admission to the obstetrical service, and these same two patients ultimately required unplanned ICU admission. Importantly, their care prior to COVID-19 diagnosis involved exposures to multiple health care workers, all of whom lacked appropriate PPE. Further, five of seven confirmed COVID-19-positive women were afebrile on initial screen, and four did not first report a cough. COVID-19 screening and testing protocols currently vary by institution, but in some locations where testing availability remains limited, the minimal symptoms reported for some of these cases might have been insufficient to prompt COVID-19 testing.
The illness can become a very big problem for both the women giving birth as, in this case, two of the seven ended up in ICU. But it also a problem for the doctors, nurses and medical personnel who are not properly outfitted with PPE and come into contact with the asymptomatic women (there were two in this case study).
The authors note: “Until adequate PPE supplies exist, we can reasonably expect our obstetrical and anesthesiology providers to become ill and exit the workforce at an accelerated rate.”
While reading about the above-mentioned research, I found another paper titled, “Why are pregnant women susceptible to COVID-19? An immunological
viewpoint” in the Journal of Reproductive Immunology. Researhers from Chicago Medical School and Wayne State collaborated to look at how pregnancy is affected by COIVD-19. Authors of this paper noted that pregnant women may be more susceptible to COVID-19 since pregnant women, in general, are vulnerable to respiratory infection. While they did mention in their abstract that there is no evidence for vertical transmission of the virus, they did mention that there was an “increased prevalence of preterm deliveries” and COVID-19 may alter immune responses at the maternal-fetal interface, and affect the well-being of mothers and infants.
…due to the characteristic immune responses during pregnancy and potential risks from the cytokine-storm by COVID-19 infection, pregnant women with COVID-19 may face severe morbidity and even mortality. Although existing evidence does not support the intrauterine vertical transmission, the maternal infection and inflammation occurred in response to COVID-19 could affect the developing fetus and even postnatal life…
Researchers were less concerned with direct transmission of the virus to the fetus and more concerned with how the illness affects the the mother. And the potential complications, both direct and indirect, that the illness could produce. But at this point there wasn’t enough data to make any sweeping conclusions.
Based on what I’ve read, though, I would guess that these researchers as well as the previous above-mentioned researchers would suggest that pregnant women do all they can to avoid contracting COVID-19.
From the World Health Organization
The WHO issued a statement concerning the world’s response to COVID-19 and the three steps countries should take to combat the virus.
The restrictions many countries have put in place to protect health are taking a heavy toll on the income of individuals and families, and the economies of communities and nations.
We are in a shared struggle to protect both lives and livelihoods.
In the short term, countries can ease the burden on their populations through social welfare programs to ensure people have food and other life essentials.
For some countries, debt relief is essential to enable them to take care of their people and avoid economic collapse. This is an area of cooperation between WHO, the IMF and the World Bank.
But ultimately, the best way for countries to end restrictions and ease their economic effects is to attack the virus, with the aggressive and comprehensive package of measures that we have spoken about many times before: find, test, isolate and treat every case, and trace every contact.
If countries rush to lift restrictions too quickly, the virus could resurge and the economic impact could be even more severe and prolonged.
Financing the health response is therefore an essential investment not just in saving lives, but in the longer-term social and economic recovery.
There are three main areas for countries to focus on.
First, we call on all countries to ensure core public health measures are fully funded, including case-finding, testing, contact tracing, collecting data, and communication and information campaigns.
Second, we also call on countries and partners to strengthen the foundations of health systems. That means health workers must be paid their salaries, and health facilities need a reliable supply of funding to purchase essential medical supplies.
Third, we call on all countries to remove financial barriers to care.
Things you should be doing now
I know this can all seem overwhelming at times. The sheer amount of information being kicked out by every media outlets is like an avalanche.
So, here are some things: Stay home if you can! Gotta work? That’s understandable. Need food? Sure, head to the store. But try to skip any “for fun” activities in public where you would be interacting with others or in a place with multiple other people.
Some CDC’s guidance:
— Know where to get your local / state-level information
For Mississippi: https://msdh.ms.gov/msdhsite/_static/14,0,420.html
For Louisiana: http://ldh.la.gov/Coronavirus/
For Alabama: http://www.alabamapublichealth.gov/infectiousdiseases/2019-coronavirus.html
If you live in a state outside of the region, head to google and type in, “dept of health” followed by whatever state you live. Google should take you to that state’s department of health and on the main page, most states have a link to an update on the Coronavirus.
— Know the Symptoms
Look for things like a fever, dry cough, and shortness of breath. But also know when it may become an emergency. It becomes an emergency when you have difficulty breathing, a persistent pain or pressure in the chest, you develop general confusion, and if you develop bluish lips or face. Also recognize that body aches, weak stomach, nasal congestion, a sore throat, and other symptoms of the regular flu are not the same as the symptoms with Coronavirus.
— Stay home when you are sick
Any kind of sick. If you feel like you may have Coronavirus, call your health care provider’s office in advance of a visit. If you have any sickness, the CDC recommends to limit movement in the community, limit visitors, and practice good social distancing.
— Know if you are at a higher risk
Know what additional measures those at higher risk and who are vulnerable should take. Those at higher risk include older adults (over 60), people who have serious chronic medical conditions (like heart disease, diabetes, lung disease). Some research has indicated that people with asthma may also be included in the higher risk category.
— Take steps to mitigate your infection
The CDC recommends to “Implement steps to prevent illness” by washing high-traffic areas more often, washing hands with soap and water and if someone is sick, to isolate the sick person into a low-traffic area of the home.
— Create a Household Plan
Create a household plan of action in case of illness in the household or disruption of daily activities due to COVID-19 in the community.